Masterclass Part One: An Introduction to Anterior Hip Replacement
Lesson Overview
The first part of the 5-part masterclass series covers the evolution of the anterior approach presented by Dr. Jonathan Yerasimides.
Anterior predates posterior as arthroplasty
The earliest mention of the approach was in an article published by a German surgeon called Karl Hueter in 1881. He described an approach to the hip joint through an internervous, intermuscular plane.
The first English description of the approach was in the US in the early 1900s, by Marius Smith-Peterson. This Boston-based surgeon was using it initially for DDH surgery, but in 1923 [1] he described this technique for a mold arthroplasty – probably the first ever description of an anterior hip arthroplasty. Interestingly, this was some time before the first descriptions of a posterior approach – which came about in the 1970s – and was then described as a southern approach.
The approach evolved further in 1950s in France, where Robert and Jean Judet described the origin of today’s anterior surgery technique – an anterior approach for an arthroplasty procedure using an acrylic head prosthesis. And there’s a direct link from these origins to the approach we use in the US today. Robert Judet trained Emile Letournel, who later became renowned for his classification of acetabular fractures, and who in turn trained, Joel Matta, the developer of the modern technique used in the US today (and founder of the Anterior Hip Foundation).
Benefits of an anterior approach
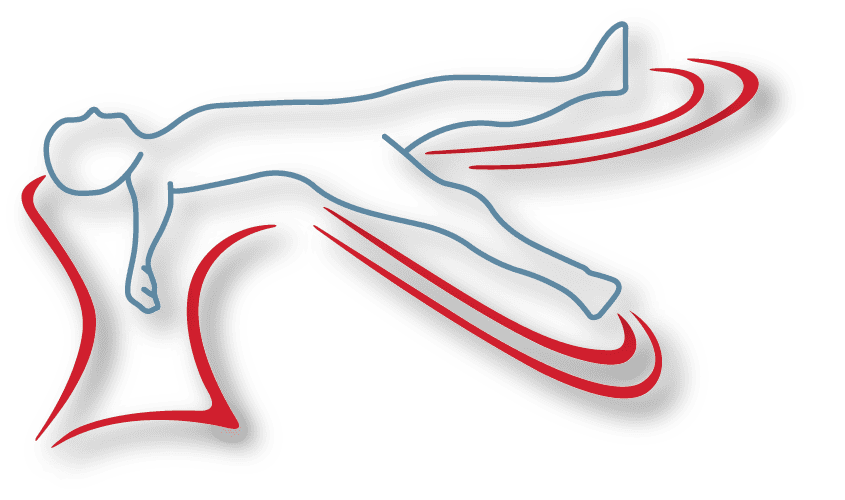
The original rationale of this approach was that the patient is in a supine position- making it easier to appreciate the positioning of the acetabular components, but there are other significant benefits. The supine positioning also makes it easier to ascertain leg lengths. It’s also worth remembering that the hip is essentially an anterior structure, so the anterior intermuscluar plane means that it is much easier to access the acetabulum.
And of course, unlike a posterior approach, the posterior capsule remains intact, which means that there are no dislocation precautions. That’s not to say that an anterior approach hip cannot dislocate, as there can still be anterior instability – but we don’t spend much time with our leg extended and externally rotated, which would be the dislocation position. We spend far more time seated, or reaching down to put on socks and shoes – making the posterior approach more naturally susceptible to dislocation.
Another advantage is the abductors are left intact. The anterolateral approach, which is also a very stable surgical approach to the hip, has the disadvantage of releasing the abductors and reattaching them which means they take time to heal, which can lead to a prolonged limp. The anterior approach keeps both the posterior capsule and abductors intact – ensuring a high degree of joint stability and fast recovery times.
There’s also the potential for a simultaneous bilateral replacement thanks to the supine position. Additionally, the position enables the use of fluoroscopy in the operating room – an easy addition that brings significant value in terms of confirming accurate positioning of the acetabular component, the position and fill of the femoral component, the leg length and the offset.
Initial Patient Selection
When you are starting out using the anterior approach, selecting the right patients will help you set yourself up for success. Your ideal initial patient is:
- Female – muscle mass makes any surgery more difficult and women tend to have less muscle mass than men
- No deformity or previous surgery
- Good bone quality
- Thin – with obese patients – the hip is of course still near the front of the body, but it is deeper compared to slimmer people. There’s more tissue to get through and femoral elevation is going to be more difficult. Crossing heavy skin creases also elevates risk for wound dehiscence because this is a high stress area. In these cases we often use a bikini incision (which we’ll explore in chapter 2). However, it is also worth noting that there’s less tissue at the front of the hip of an obese patient compared to a posterior approach.
High Risk Patients
There are some other high-risk patients you may want to avoid initially – (however when you have experience, these are the patients who benefit the most). These include those with neuromuscular disease, cognitive impairment or DDH.
What to look out for on pre-operative X-rays.
The first and simplest thing to consider is the width of the pelvis. Draw a plumb line through the diaphysis of the femur straight up – and look where that line crosses the iliac crest. An iliac crest that overhangs that line is going to make surgery more challenging as, with an anterior approach, we have to clear the iliac crest in order to broach the femur.
On the femoral side, there are some other things to look out for:
The longer the femoral neck and the more valgus the femoral neck, the easier the surgery – and conversely, the more varus and shorter the femoral neck, the more difficult it’s going to be due to the length of the hip capsule. To elevate the femur, we must get the femur lateral to and away from the acetabulum. When you initially externally rotate and try to drop or adduct the leg, the tip of the trochanter gets caught behind the acetabulum. A shorter femoral neck, with its tighter hip capsule makes it more challenging to get the femur lateralized to clear the acetabulum. A long neck corresponds to a long capsule which means good femoral mobility and easier access.
Spino-pelvic considerations
There’s been a lot of focus on the spino-pelvic relationship recently as it can have implications for cup positioning. A normal spine transitions to a posterior pelvic tilt when moving to a sitting position – which allows the femoral neck to clear the anterior acetabulum. However, patients who have lost the natural lordosis in their lumbar spine, for example after fusion surgery, are unable to change the position of their pelvis from standing to sitting. This results in anterior impingement of the artificial hip and risk of posterior dislocation. That’s why this relationship is particularly important with a posterior approach, as the surgical approach already creates posterior instability.
In the OR, this means that for a patient with a stiff lumber spine you will need to add anteversion to prevent impingement when sitting. You also want to ensure bony anterior coverage with no cup overhang at the anterior acetabulum as this will lead to iliopsoas impingement, iliopsoas tendinitis and pain.
The Smith Peterson/Hueter approach Step by Step
The Masterclass also includes a step by step walk through of the Smith Peterson/Hueter approach surgery starting from the location of the incision, and considerations for different table types. This includes a detailed overview of relevant anatomy, superficial and deep dissection, how to idenfy and ligate the lateral femoral circumflex vessels, performing the capsulotomy, osteotomy, acetabular exposure and preparation, cup insertion, and femoral exposure.
Click here for the second part of the Masterclass: Considerations, Tips and Tricks for a Primary Hip Arthroplasty.