Anterior Hip Replacement: Benefits, Recovery, and What Patients Should Know
If You’re Here, You’re Probably Looking for Answers
If you’ve landed on this page, chances are you—or someone you care about—has been told they may need a hip replacement.
Hip replacement is one of the most successful procedures in modern medicine, and the information about different approaches and technologies can be overwhelming. But understanding these options can help you have a more informed, confident conversation with your surgeon.
This guide explains the anterior approach to hip replacement, what it is, where it came from, and why it may be recommended for some patients.
A Commitment to Education and Evidence
Understanding Hip Replacement Surgical Approaches
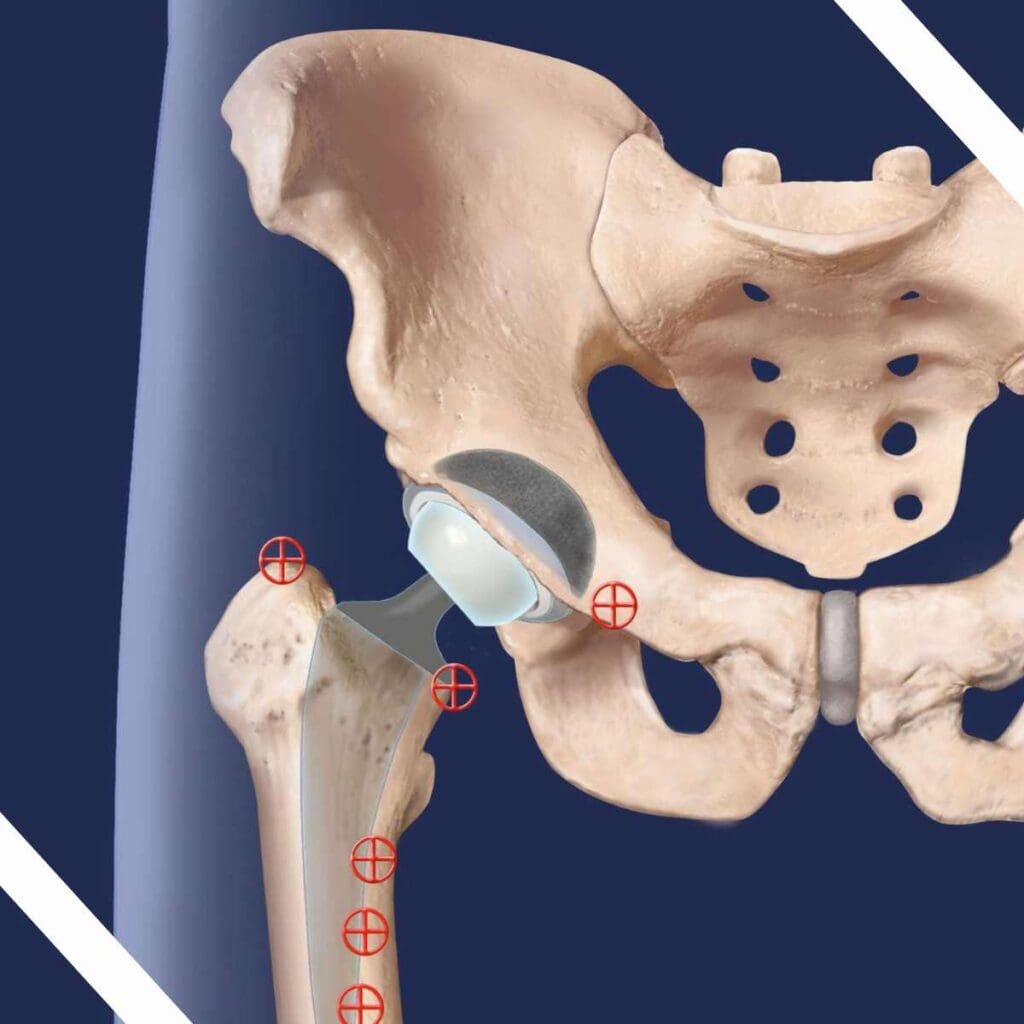
In total hip replacement, the damaged hip joint is replaced with artificial components designed to relieve pain and restore mobility. The implant itself is similar across techniques - the difference lies in how the surgeon accesses the joint.
The most common hip replacement approaches include:
- Posterior approach (from the back of the hip)
- Lateral or anterolateral approach (from the side of the hip)
- Anterior approach (from the front of the hip)
Each approach has advantages and considerations. The anterior approach is distinct because it allows the surgeon to reach the hip joint by working between muscles, rather than cutting or detaching them.
The History of the Anterior Approach: An Established Technique with Deep Roots
The anterior approach to hip replacement is not new.
The first hip replacement performed through an anterior approach was carried out in 1947 in Paris by Robert Judet, with his son Thierry Judet continuing the practice. Decades later, in 1981, Joel Matta traveled to Paris to study pelvic and acetabular surgery, where he learned the anterior technique.
Although he initially focused on fracture surgery, Dr. Matta revisited the anterior approach in the mid-1990s after seeing successful patient outcomes. He went on to refine, standardize, and teach the technique in the United States, training generations of surgeons who are now leaders in hip replacement surgery.
Dr. Matta also founded the Anterior Hip Foundation to advance surgeon education, research, and best practices related to the anterior approach.
Read more about Joel Matta’s journey in this series of blog posts:
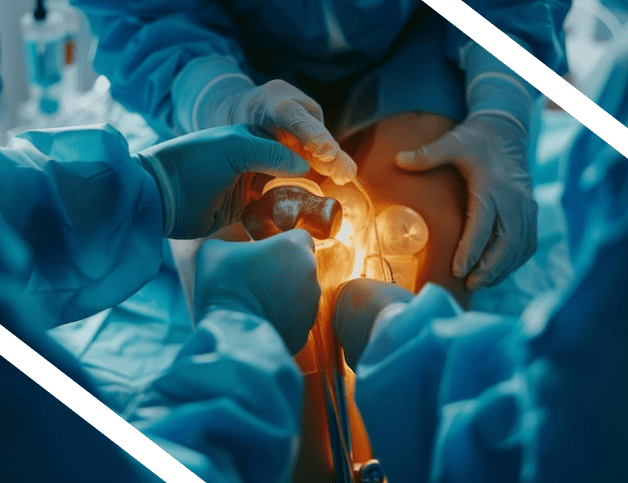
How the Anterior Approach Works
At its core, the anterior approach is designed to preserve the body’s natural anatomy while restoring hip function.
Key features include:
- A skin incision typically about 4 inches long on the front of the hip (either vertical or a horizontal “bikini” incision)
- Slight variation in incision length based on patient anatomy
- Access to the hip joint through a natural interval between muscles
- Preservation of all major muscle attachments to the femur
This approach is possible because the hip joint lies closer to the skin at the front of the body and is covered by a thinner layer of muscle and soft tissue than from the side or back.
Benefits of the Anterior Approach to Hip Replacement
When performed by an experienced surgeon, the anterior approach may offer several meaningful benefits for patients.
Muscle Preservation
Unlike posterior and anterolateral approaches, which require cutting or detaching muscles, the anterior approach preserves important muscle groups. This matters because the artificial hip depends on surrounding muscles for strength, stability, and movement
Immediate Stability and Lower Risk of Dislocation
Because muscles are left intact, the hip is typically stable immediately after surgery.
This can result in:
A lower risk of dislocation
No routine post-operative hip precautions
No mandatory elevated toilet seats or special chairs
Freedom to bend, twist, cross legs, and move naturally
Dislocation after hip replacement is rare, but when it occurs it is extremely painful and often requires emergency medical treatment. Preserving stabilizing muscles helps reduce this risk.
Faster Early Recovery
Avoiding cutting or detaching muscles can enable:
Walking the day of surgery
Immediate full weight-bearing
In many U.S. centers, same-day discharge
Formal physical therapy is often minimal. Walking and everyday activity are usually sufficient, with outpatient therapy available if needed.
Accurate Implant Positioning and Leg Length
During anterior hip replacement, patients lie on their back (supine position). This allows surgeons to use real-time imaging (fluoroscopy) during surgery to:
Assess leg length
Optimize implant size and position
Improve alignment and long-term function
Leg length differences have historically been a challenge in hip replacement surgery. Intraoperative imaging helps surgeons address this more reliably.
Why Isn’t the Anterior Approach Used Everywhere?
The anterior approach has a significant learning curve.
It is technically demanding
Requires specialized training and equipment
Studies suggest surgeons may need 100 or more cases to become proficient
The benefits of the approach mean that its use is growing significantly. In the USA in 2010, only about 12% of U.S. surgeons performed anterior hip replacement. By 2023, that number had grown to more than 50%, reflecting expanded training and education.
When performed by a well-trained surgeon, complication rates are comparable to traditional hip replacement approaches, and there is no evidence of increased nerve injury risk.
Questions to Ask Your Surgeon About Hip Replacement
These questions can help guide an informed discussion with your surgeon:
- What surgical approach do you recommend for me, and why?
- How often do you perform the anterior approach to hip replacement?
- What is your experience and training with this approach?
- What does recovery typically look like for your patients?
- Will I have movement restrictions after surgery?
- How do you manage leg length and implant positioning during surgery?
- What risks should I be aware of, and how are complications handled?
- Am I a candidate for same-day or short-stay discharge?
- What anaesthesia can I expect? Spinal and sedation or a general anaesthesia?
- If I schedule surgery, what do the timelines look like? eg when should I expect to have tests, return for a pre-op visit?
- What can I do to prepare for surgery? Do you recommend pre-hab exercises, nutrition plans?