Masterclass #3: Advanced Techniques in Anterior Hip Replacement
Welcome to the third lecture in our direct anterior approach hip arthroplasty masterclass series. In this session, Dr. Yerasimides covers more advanced topics that include not just the surgical technique, but also some invaluable tips on how to interpret X-rays to ensure the best possible outcomes.
He shares how this approach is not just appropriate for primary hip replacement surgeries, it is actually a very versatile approach for revisions. We know that it gives an excellent exposure of the acetabulum, including the inner table of the pelvis, and can also be used for large femoral defects down to the knee.
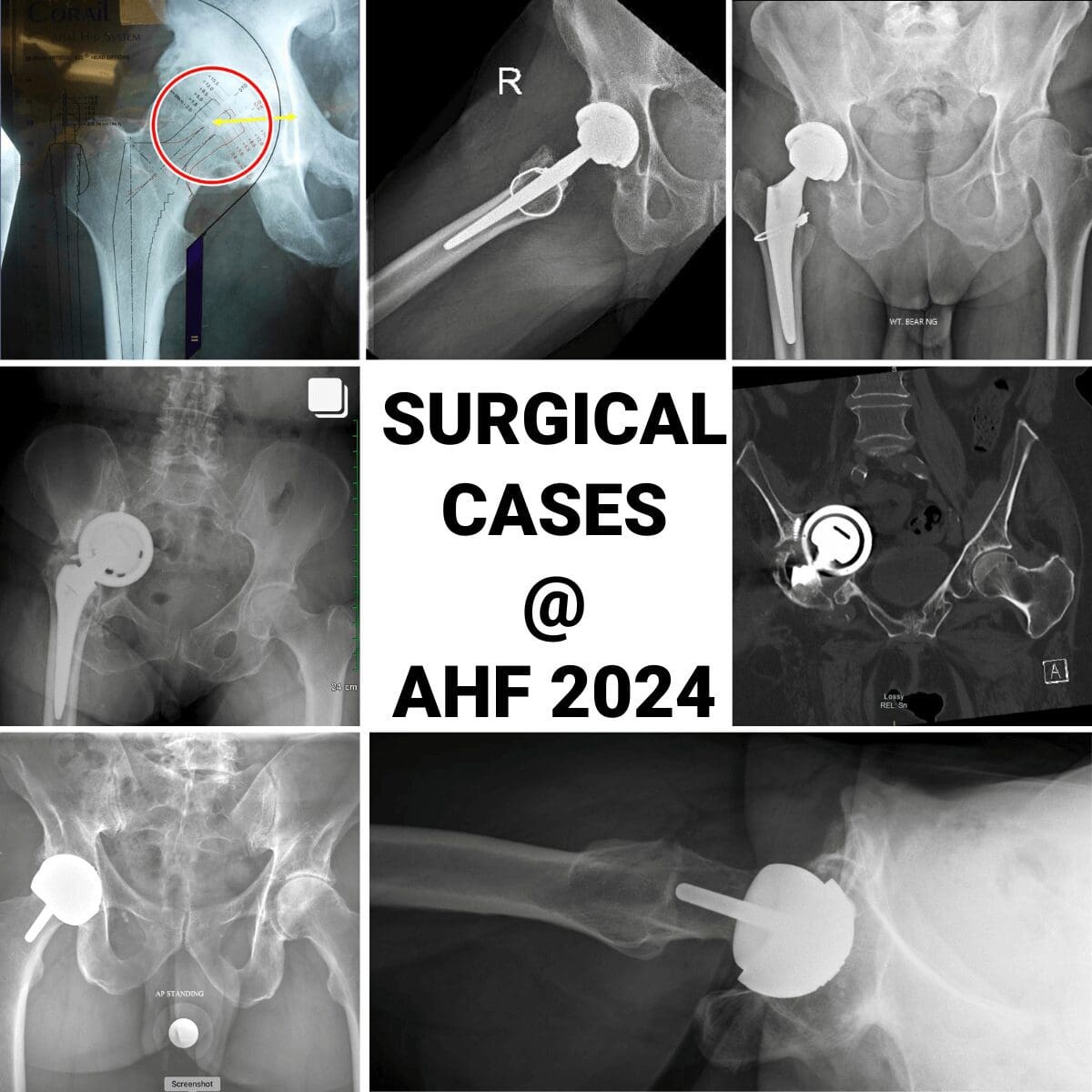
X-Rays
We know the AP pelvis view we get with fluoroscopy in the OR during an anterior approach is valuable as we can interpret characteristics such as leg length, offset and pelvic tilt. Dr. Yerasimides shares some tips and tricks for getting the most information out of this simple two-dimensional image and what it tells you about the three dimensional pelvis. This understanding is particularly valuable when you are dealing with issues that may require revision surgery – such as loose cups and migration.
One thing to bear in mind from the outset is that you need to ensure that the image you are looking at is in the right plane- which means you want to make sure that the pelvis is perfectly parallel to the floor and the C-arm. An easy way to identify this is to look at the relationship between the ilioischial line and the teardrop on each side – to check that they are equal. Remember, you want to tilt the table not he C-arm to address any rotation – tilt the table towards the side where the ilioischial line is more lateral to the teardrop.
Dr. Yerasimides also addresses pelvic tilt, how to identify loss of lumbar lordosis, the challenges associated with loss of spinal mobility and how it affects the appropriate anteversion of the cup.
Planning your incision
Your incision location should be located slightly differently depending on whether you are using a standard OR table or a specialized orthopedic table. The difference is not as crucial for a primary total hip, however when it comes to revisions and the associated long straight instrumentation, for example cement removal tools or long stems, the placement of the incision becomes much more important.
Dr. Yerasimides shares details of the Hana table he uses – where the femur is in pure extension while it is being prepared as the leg drops straight down to the floor with little adduction. That means that with this table, the incision needs to be more anterior to protect the skin when using those straight instruments.
On a standard Orthopedic operating table, when the femur is being prepared, it is in pure adduction as we lift the opposite leg and tuck the operative leg under it. Some surgeons extend the bottom of the table but this gives maybe 15 or 20 degrees of extension at the most. This means that the orientation of the bone preparation is more from an anterolateral position, which means that the skin incision needs to be more lateral.
You also want your primary incision to be extensible. On the Hana table with the femur in extension, when you are performing a femoral revision, the incision should run in a straight line proximally, not curving along the iliac crest. This is not for additional exposure but to protect the skin from the straight reamers.
Anterior Revisions
When Dr. Yerasimides first started in private practice after his training, the anterior approach was generally considered suitable for primary hips and wasn’t perceived as being an extensile approach appropriate for revisions. Since that time, he has undertaken arguably more anterior revisions in the US than anyone else and can attest to the fact that the anterior approach is in fact extremely extensile on the femoral side.
In fact, once you have understand all the femoral mobilizations, there are no limitations for femoral revisions – as you have exposure all the way to the knee. The only limiting factor for anterior approach revisions are large posterior wall or posterior column defects on the acetabular side. You have good visibility of the area, but it can be difficult to get screw orientation into the augments. Today, retroacetabular bone loss that requires an augment is the only reason that Dr. Yerasimides would use a posterior approach.
He also touches on a technique for addressing Paprosky 3B defects that would typically be fixed with a cup and cage or a tri-flange device. Dr. Yersasimides has reconstructed the anterior acetabulum with the same concept as the posterior acetabulum – it involves operating on the inner table of the pelvis and implanting augments. Since 2011 he has performed approximately 22 to 25 of these surgeries and so far the results have been excellent.
The bikini Incision
The masterclass also covers the bikini incision, an advanced technique that is becoming more and more popular. Dr. Yerasimides started using this incision for very morbidly obese patients with heavy skin creases and skin folds. In the past 1-2 years, he has expanded to using this incision on approximately 60-70% of cases. We know that if we make anterior incisions across that skin fold it represents a very high risk for wound breakdown. By making the incision horizontal in the bikini line, patients heal incredibly fast and well as there’s no stress on the incision. Of course, the other case for using a bikini incision is for cosmetic reasons in young patients, particularly females who don’t want an ugly scar.
It is an advanced technique, particularly for bigger patients but the value of healing the skin is more important than saving an extra five or ten minutes in the operating room.
The masterclass also includes a step by step video of a bikini incision.
Check out Part four, which focuses on Acetabular Revisions here.